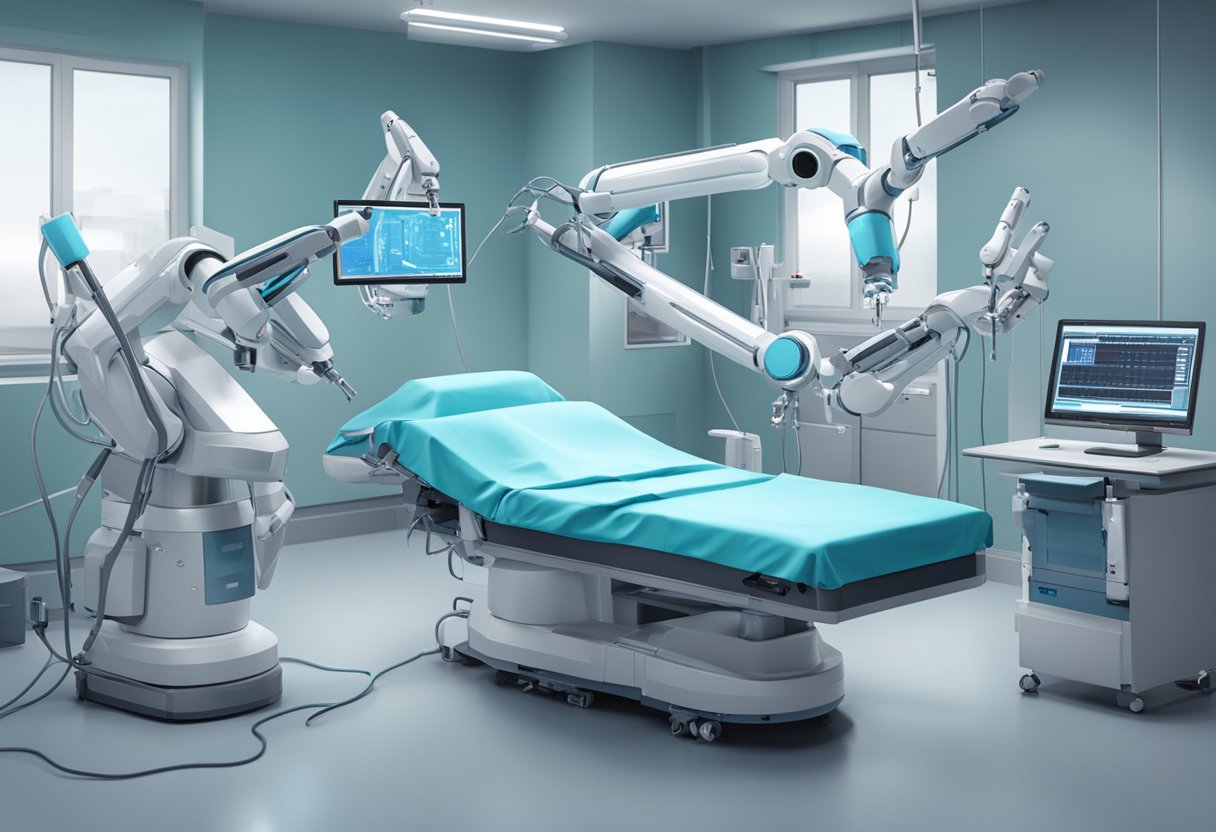
Advances in robotic surgery have revolutionized the field of medicine in recent years.
Robotic surgical systems are equipped with robotic arms that can rotate 360 degrees and mimic the natural movements of a surgeon’s hand but with significantly enhanced dexterity.
The robotic arms’ stability and precision reduce the risk of errors during surgery, leading to improved patient outcomes and reduced postoperative complications.
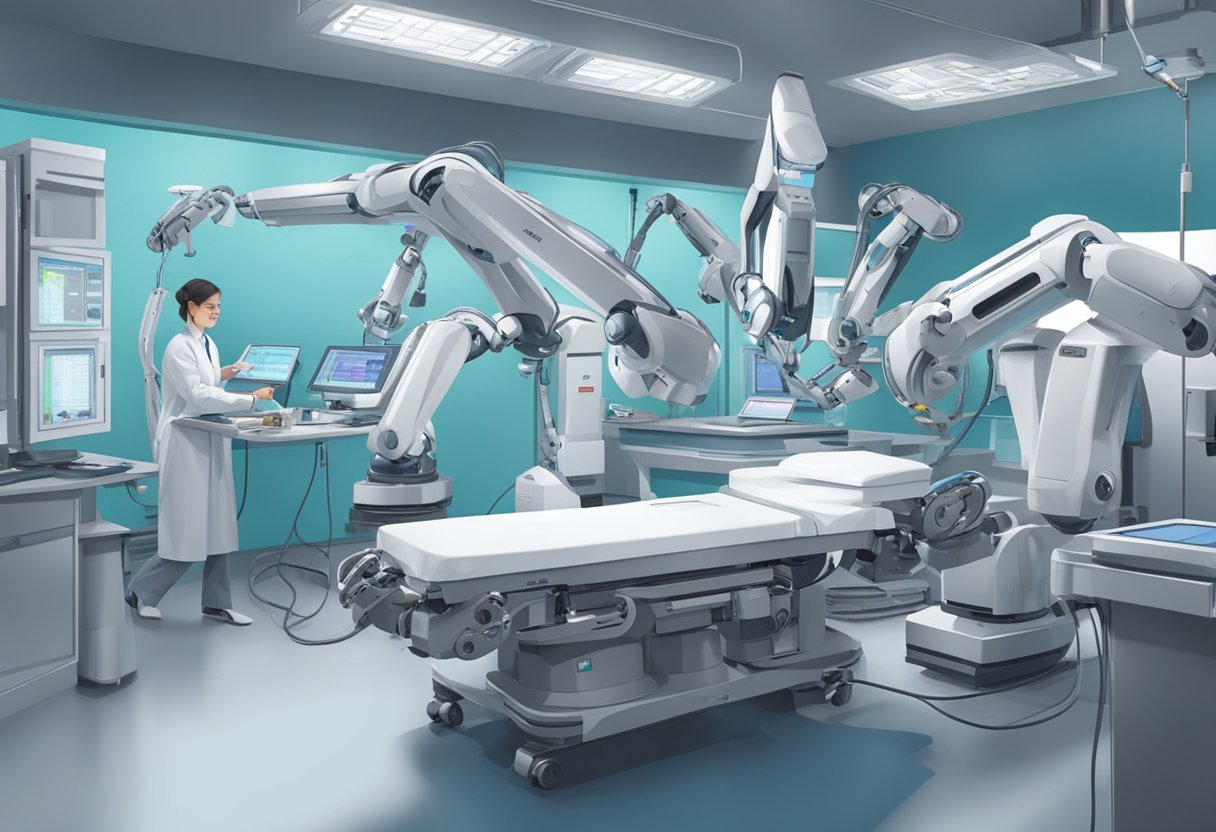
The evolution of robotic surgery has been remarkable, with the introduction of the da Vinci system being a significant milestone.
The da Vinci system consists of a console from which the surgeon remotely controls arms connected to a robotic cart beside the patient.
A dual-camera endoscope mounted on one arm transmits images of the surgical field to the console, providing the surgeon with a magnified three-dimensional (3D) view.
This has enabled surgeons to perform complex procedures with greater accuracy and efficiency, resulting in better patient outcomes.
Key Takeaways
- Advances in robotic surgery have led to improved patient outcomes and reduced postoperative complications.
- The introduction of the da Vinci system has been a significant milestone in the evolution of robotic surgery.
- Robotic surgery enables surgeons to perform complex procedures with greater accuracy and efficiency.
Evolution of Robotic Surgery
Origins and Historical Milestones
Robotic-assisted surgery has come a long way since its inception in the 1980s.
The origins of robotic surgery can be traced back to the development of the first surgical robot, the PUMA 560, which was used to perform a neurosurgical biopsy in 1985.
The PUMA 560 was designed to assist in surgical procedures by providing precision and accuracy in movements that are difficult to achieve with the human hand.
In 1999, the da Vinci Surgical System was introduced, which revolutionized the field of robotic-assisted surgery.
The da Vinci system allowed surgeons to perform minimally invasive surgeries with greater precision and control.
The system consists of a console that the surgeon sits at, a patient-side cart with four robotic arms, and a 3D high-definition vision system.
The surgeon controls the robotic arms from the console, which translates their hand movements into precise movements of the surgical instruments.
Since the introduction of the da Vinci system, there has been a significant increase in the use of robotic-assisted surgery.
The system has been used in a wide range of procedures, including urological, gynecological, and gastrointestinal surgeries.
The da Vinci system has also been used in cardiac surgery, thoracic surgery, and head and neck surgery.
Current State of Robotic Surgical Systems
Today, there are several robotic surgical systems available in the market, including the da Vinci Xi, the Senhance Surgical System, and the Versius Surgical System.
These systems have improved upon the original da Vinci system, offering greater precision and control, as well as smaller and more flexible instruments.
Technological Advancements in Robotic Surgery
Recent years have seen significant advances in robotic surgery technology, resulting in improved patient outcomes.
This section will explore some of the latest technological advancements in robotic surgery, including haptic feedback and sensory integration, artificial intelligence and machine learning, and augmented reality and enhanced visualization.
Haptic Feedback and Sensory Integration
Haptic feedback is an essential component of robotic surgery, as it allows the surgeon to feel the tissues being operated on.
This feedback is provided through a variety of sensors and actuators that are integrated into the robotic system.
The integration of haptic feedback into robotic surgery has been shown to improve surgical precision and reduce the risk of complications.
Sensory integration is another critical aspect of robotic surgery.
It refers to the integration of visual, auditory, and tactile information to provide the surgeon with a more comprehensive understanding of the surgical site.
The use of sensory integration in robotic surgery has been shown to improve surgical outcomes and reduce the risk of complications.
Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are rapidly transforming the field of robotic surgery.
AI and ML algorithms can analyze vast amounts of data to identify patterns and predict outcomes.
This technology can be used to assist the surgeon in making decisions and to optimize the surgical process.
One of the most promising applications of AI and ML in robotic surgery is the development of predictive models.
These models can be used to predict the likelihood of complications and to identify patients who are at high risk of developing complications.
This information can then be used to develop personalized treatment plans that are tailored to the individual patient.
Augmented Reality and Enhanced Visualization
Augmented reality (AR) and enhanced visualization technologies are also transforming the field of robotic surgery.
AR technology can be used to overlay virtual images onto the surgical site, providing the surgeon with a more comprehensive view of the surgical site.
This technology can be used to improve surgical precision and reduce the risk of complications.
Enhanced visualization technologies, such as high-definition cameras and 3D imaging, are also improving the surgical process.
These technologies provide the surgeon with a more detailed view of the surgical site, allowing for more precise surgical maneuvers and reducing the risk of complications.
Clinical Applications and Outcomes

Robotic surgery has revolutionized the practice of surgery, providing improved precision and accuracy in minimally invasive procedures. This has resulted in better clinical outcomes for patients across multiple specialties, including urology, gynecology, and oncology.
Specialty-Specific Outcomes
In urology, robotic surgery has been shown to reduce blood loss, shorten hospital stays, and improve functional outcomes compared to traditional open surgery.
In gynecology, robotic surgery has been associated with lower rates of complications, reduced pain, and faster recovery times compared to laparoscopic surgery.
In oncology, robotic surgery has been shown to be as safe and effective as traditional open surgery, while providing the added benefits of smaller incisions and faster recovery times.
Comparative Studies and Randomized Trials
Several randomized controlled trials have compared robotic surgery to traditional open surgery and laparoscopic surgery, with generally favorable results for robotic surgery.
A meta-analysis of 24 studies found that robotic surgery was associated with lower rates of complications, shorter hospital stays, and faster recovery times compared to open surgery.
Another meta-analysis of 14 studies found that robotic surgery was associated with lower rates of complications and shorter hospital stays compared to laparoscopic surgery.
Economic Impact and Cost-Effectiveness
Assessing the Costs of Robotic Surgery
Robotic surgery is a relatively new technique that has been shown to improve patient outcomes in a variety of procedures. However, the high cost of robotic systems has been a barrier to its widespread adoption, particularly in low- and middle-income countries.
The cost of a robotic system can range from $1 million to $2.5 million, and the cost of each procedure can be up to 40% higher than traditional surgery.
Despite the higher up-front costs of robotic surgery, some studies have shown that it can be cost-effective in the long run.
For example, a study by Menger et al found that robotic technology can save time, reduce revision rates, and improve accuracy, resulting in cost savings and enhanced patient care.
Additionally, Bai et al conducted a comprehensive review of 31 cost-utility analyses and suggested that robotic surgery is generally more cost-effective than open surgery in a variety of procedures.
Cost-Benefit Analysis in Different Regions
The economic impact of robotic surgery can vary widely depending on the region and the specific procedure.
In high-income countries, the cost-effectiveness of robotic surgery may be more easily justified due to higher healthcare costs and greater access to technology.
However, in low- and middle-income countries, the high cost of robotic systems may be a significant barrier to its adoption.
To assess the cost-effectiveness of robotic surgery in different regions, cost-benefit analyses must be conducted that take into account the specific costs and benefits of the technology in each context.
These analyses should consider not only the direct costs of the robotic system and each procedure, but also the indirect costs, such as the impact on patient outcomes and quality of life.
Challenges and Future Perspectives

Overcoming the Learning Curve
One of the biggest challenges in robotic surgery is the steep learning curve.
Surgeons need to undergo extensive training to become proficient in using the robotic system.
This requires a significant investment of time and resources, both for the surgeon and the hospital.
Moreover, the lack of standardized training programs and certification processes can lead to variability in outcomes and patient safety.
To overcome this challenge, healthcare institutions need to establish standardized training programs that incorporate simulation and hands-on training.
This will not only improve the proficiency of the surgeon but also ensure patient safety and better outcomes.
Ethical and Legal Considerations
As with any new healthcare innovation, robotic surgery raises ethical and legal considerations.
The use of robots in surgery raises questions about the role of the surgeon, the responsibility for errors, and the impact on the doctor-patient relationship.
To address these concerns, healthcare institutions need to establish clear guidelines and protocols for the use of robotic surgery.
This includes informed consent, patient education, and a clear understanding of the risks and benefits of the procedure.
Future Innovations and Directions
The future of robotic surgery holds great promise. Advancements in technology such as haptic feedback, augmented reality, and artificial intelligence will improve the precision and accuracy of surgical procedures.
Moreover, the integration of robotic surgery with other healthcare innovations such as telemedicine and remote monitoring will enable better patient outcomes and access to care.
However, to realize the full potential of robotic surgery, healthcare institutions need to continue to invest in research and development. This includes the development of new robotic systems, the establishment of standardized training programs, and the integration of robotic surgery with other healthcare innovations.